Differences Between Subcutaneous and Visceral Adipose Tissue
Understanding the anatomical and functional characteristics of abdominal fat compartments.
Anatomical Compartmentalization
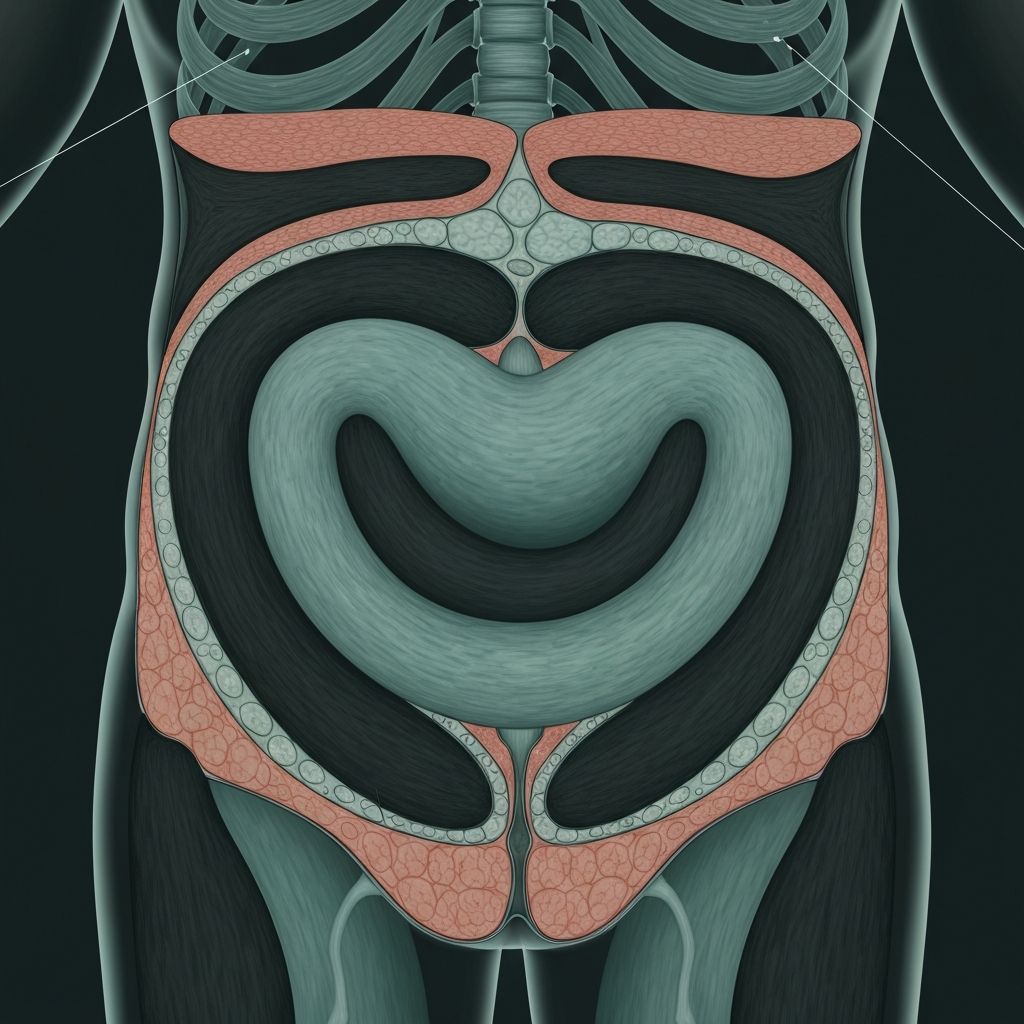
The abdominal region contains two distinct adipose tissue compartments with fundamentally different anatomical locations and tissue characteristics. Subcutaneous adipose tissue comprises the fat layer located directly beneath the skin (hypodermis) and superficial to the abdominal musculature (rectus abdominis and external oblique muscles). This compartment is readily accessible to the surface and represents the most visible fat accumulation.
Visceral adipose tissue, by contrast, occupies the peritoneal cavity, surrounding internal organs including the liver, pancreas, kidneys, and intestines. This compartment is deep to the abdominal muscles and directly adjacent to organ systems. The omentum majus (greater omentum) represents a substantial visceral fat depot that drapes over the intestines.
Metabolic Properties
Despite occupying the same general anatomical region, these compartments demonstrate markedly different metabolic characteristics. Visceral adipose tissue exhibits significantly higher metabolic activity and turnover rates compared to subcutaneous reserves. This elevated activity reflects:
- Greater lipoprotein lipase activity (enzyme regulating fatty acid uptake)
- Higher rates of lipid mobilization and free fatty acid release
- More dynamic hormone-sensitive lipase expression
- Enhanced insulin-stimulated glucose uptake
- Greater sensitivity to hormonal signaling (insulin, glucagon, catecholamines)
These differences mean visceral fat responds more rapidly to hormonal and metabolic signals, both accumulating during periods of energy surplus and mobilizing during caloric deficit more readily than subcutaneous stores.
Endocrine and Inflammatory Function
Visceral adipose tissue functions as a more active endocrine organ than subcutaneous fat. It produces substantially higher concentrations of pro-inflammatory cytokines including:
| Cytokine | Visceral Adipose Tissue | Subcutaneous Adipose Tissue |
|---|---|---|
| Interleukin-6 (IL-6) | Elevated production | Lower baseline levels |
| Tumor Necrosis Factor-α (TNF-α) | High concentrations | Minimal production |
| Monocyte Chemoattractant Protein-1 | Elevated | Lower levels |
| Plasminogen Activator Inhibitor-1 | High expression | Low expression |
This chronic inflammatory state in visceral adiposity has significant metabolic consequences, contributing to systemic inflammation markers and altered insulin sensitivity.
Portal Vascular Drainage
A critical physiological distinction involves vascular drainage patterns. Visceral adipose tissue drains directly into the portal circulation via the portal vein, delivering free fatty acids and adipokines directly to the liver before systemic distribution. Subcutaneous fat, conversely, drains into systemic venous circulation, bypassing the liver initially.
This anatomical difference has profound metabolic implications. Portal delivery of elevated free fatty acids to hepatic tissue promotes hepatic lipid accumulation, triglyceride synthesis, and altered glucose metabolism. Subcutaneous fat mobilization, reaching the liver through systemic circulation, produces different metabolic effects on hepatic function.
Adipokine Secretion Patterns
The two compartments demonstrate distinctly different adipokine production profiles:
Adiponectin, an adipokine with insulin-sensitizing and anti-inflammatory properties, is produced at significantly lower concentrations by visceral fat compared to subcutaneous depots. Leptin, the satiety hormone, demonstrates dysregulated signaling in visceral obesity despite elevated absolute concentrations, contributing to leptin resistance and impaired appetite regulation.
Cellular Composition
Histological examination reveals differences in adipocyte size distribution and composition. Visceral adipose tissue typically contains larger adipocytes (hypertrophied fat cells) compared to subcutaneous compartments. This hypertrophy correlates with greater dysfunction and inflammatory activity. Visceral depots also demonstrate higher macrophage infiltration and immune cell content, contributing to elevated inflammatory tone.
Response to Metabolic Signals
The two compartments respond differently to nutritional and hormonal challenges. During periods of overfeeding, visceral adiposity preferentially expands before subcutaneous compartments in some individuals. Conversely, during caloric deficit or weight loss, visceral fat often mobilizes preferentially while subcutaneous reserves persist longer. This differential responsiveness reflects distinct gene expression patterns and hormone receptor densities between compartments.
Clinical and Research Significance
Understanding these compartment-specific differences clarifies why visceral adiposity demonstrates stronger associations with metabolic dysfunction, cardiovascular risk, and systemic inflammation compared to subcutaneous fat. Identical total body fat mass can produce different metabolic and health implications depending on the distribution between compartments.
Waist circumference measurements, while imperfect, provide clinical utility partly because abdominal measurements capture visceral accumulation more sensitively than hip or other regional measurements. Advanced imaging (CT, MRI) can distinguish visceral from subcutaneous volume, providing more precise assessment but requiring specialized equipment.
Educational Note
This article explains anatomical and physiological characteristics of adipose tissue compartments. Individual fat distribution patterns vary substantially, and compartment-specific physiology interacts with numerous genetic, hormonal, and environmental factors. This information is educational only and does not constitute medical or nutritional guidance.